Acronyms and definitions
- AGA - American Gastroenterological Association
- BMI - Body mass index
- BPD/DS - Biliopancreatic diversion with duodenal switch
- Calories and kilocalories - In the context of food, these terms are interchangeable
- Carb - Carbohydrate
- GI - Glycemic index
- IF - Intermittent fasting
- IGB - Intragastric balloon
- NHLBI - National Heart Lung and Blood Institute
- RCT - Randomized controlled trial
- 1 kg = 2.2 lbs
IMPORTANT POINTS ABOUT WEIGHT LOSS
- Do not diet! - unfortunately, people often refer to healthy eating and weight loss as "going on a diet," implying it's a temporary measure to be stopped when they "go off a diet." The truth is achieving and maintaining a healthy weight means changing eating habits forever. Simply "going on a diet" for a set length of time with the mindset that it is punishment for past overeating will inevitably lead to failure. People who are serious about their emotional and physical health do not go on diets - they adopt healthy eating habits for life.
- Forget easy answers. They do not exist. - it's been said you will never go broke selling people easy answers, and nothing could be more true when it comes to weight loss. Billions of dollars are wasted every year on quick weight-loss diets, pills, potions, injections, creams, procedures, and promises. If you are ever tempted to fall for the next diet fad or product, ask yourself one question, "If it really worked, wouldn't everyone be skinny?"
- You are overweight because you consume more calories than you burn. - many overweight people assume they can't lose weight because they are different or something is wrong with them. The reality is we are all bound by the laws of physics, which only allow us to gain matter when we consume more energy than we burn.
STEPS TO WEIGHT LOSS
- 1. Determine your normal body weight
- The most widely used measure is the body mass index (BMI)
- 2. Calculate your caloric needs
- Caloric needs are based on body weight and activity level. The links below offer several methods for calculating daily caloric needs.
- Detailed method - guide to calculating daily calorie requirements that incorporates time spent on specific activities
- Simple method - guide to calculating daily calorie requirements that uses a rough estimate of activity level
- Calorie calculator - calculator for determining the number of calories burned in a day based on activities performed
- 3. Calculate how many calories you should consume to lose weight
- Once you have figured out how many calories you use in a day, you will need to consume a deficit to lose weight
- In general, the following is true:
- A 500-calorie-a-day deficit for 7 days will lead to 1 pound of weight loss
- A 1000-calorie-a-day deficit for 7 days will lead to 2 pounds of weight loss, and so on
- Example:
- Tom calculates that he burns 2500 calories in a typical day
- If Tom consumes 2000 calories a day (500-calorie deficit) for one week, he can expect to lose 1 pound
- If Tom consumes 1500 calories a day (1000-calorie deficit) for one week, he can expect to lose 2 pounds
- Things to keep in mind:
- Exercise will greatly enhance your ability to achieve a caloric deficit
- As you lose weight, your basal energy expenditure will decrease, and you will have to increase activity and/or reduce calories to continue to lose weight
- 4. Avoid extreme eating habits and fads
- Diet fads and extreme eating habits rarely lead to prolonged, meaningful weight loss
- No diet will "trick" your metabolism or lead to miraculous, enhanced weight loss
- Reviews of some popular diets are presented below
- 5. Calories, calories, calories!
- Diet theories come and go. For years, we vilified fat, then it was carbohydrates. Despite all this, studies have consistently shown that overall calorie consumption (regardless of the source) and energy expenditure are the main determinants of weight.
- Every weight loss plan should begin and end with monitoring the number of calories consumed
- It is easier today than ever to monitor calorie intake with food packaging guidelines and new laws that require restaurants to list calories
- 6. Know what you eat
- Read labels on everything you eat, including dressings, spreads, butter, creams, etc. You will be surprised to learn how many calories you may be adding to some foods.
- Replace high-calorie foods with low-calorie alternatives or reduce their intake
- A review of the different macronutrients can be found here - fats, carbohydrates, and protein
- 7. Know how much you eat
- People who are serious about weight loss should buy a food scale and measure their serving sizes
- Portion control is an important part of weight loss. If you pour a big bowl of cereal or eat chips out of a bag, you may be getting 3 - 5 servings and 500 calories. Look at the label on what you are about to eat and weigh out a serving so that you know exactly where your calories are coming from.
- 8. Individualize your plan
- Diet programs come in all shapes and sizes, but costs, food preparation time, and palatability can make them difficult to maintain. Tailor your diet around foods you like and are willing to prepare. You do not have to give up foods you enjoy if you control your serving sizes and stay within your calorie goals.
BODY MASS INDEX (BMI)
- Normal body weight
- The first step in weight loss is determining an appropriate body weight. While an individual's perception of normal body weight is shaped by culture, environment, family, and friends, healthcare professionals categorize body weight based on mortality and disease risk. The most widely used method is the body mass index or BMI, a ratio of weight to height. While the BMI isn't perfect, studies have consistently shown it correlates well with disease risk and mortality.
- Normal weight ranges based on the BMI can be found by looking at a BMI chart - BMI chart (pdf)
- BMI calculators and charts are available at these links:
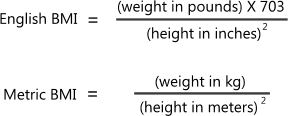
- The formula for calculating the BMI is as follows:
| BMI Categories | |
|---|---|
| Category | BMI |
| Underweight | < 18.5 |
| Normal weight | 18.5 - 24.9 |
| Overweight | 25 - 29.9 |
| Obese | 30 - 39.9 |
| Morbidly obese | ≥ 40 |
- BMI advantages
- The BMI is cheap, easy to measure, and has little interobserver variability
- It is a strong predictor of disease risk and mortality and performs well when compared to other body composition measures [1,2,3,4,5,6,7,8,9,12]
- BMI weaknesses
- Muscle mass
- The BMI cannot differentiate between muscle and fat, causing people with above-average muscle mass (e.g. weightlifters) to have higher BMIs that do not accurately reflect disease risk
- Elderly patients
- Some studies have found that elderly patients in the overweight range have lower mortality than normal-weight subjects [10,11]
- Ethnicity
- Some ethnicities have more muscle mass (e.g. Blacks) than others, altering the association between disease risk and BMI [13,14]
LOW-CARB VS LOW-FAT DIETS
- Overview
- In the eighties and nineties, low-fat diets were popular. Then the pendulum shifted, and low-carb diets became the rage with the rediscovery of the Atkins diet. Four trials comparing low-carb to low-fat diets are detailed below, along with two meta-analyses on the topic.
RCT
Low-Fat vs Low-Carb Diet for Weight Loss Over 12 Months, JAMA (2018) [PubMed abstract]
- A trial in the JAMA enrolled 609 overweight adults without diabetes
Main inclusion criteria
- Age 18 - 50 years
- BMI 28 - 40
Main exclusion criteria
- Diabetes
- Uncontrolled hypertension
- Taking medication known to affect body weight
Baseline characteristics
- Average age - 40 years
- Average BMI - 33
- Average weight - 213 lbs (97 kg)
Patients were randomized to one of two groups:
- Group 1 (305 patients): Low-fat diet (study average: carb 48%, fat 29%, protein 21%)
- Group 2 (304 patients): Low-carbohydrate diet (study average: carb 30%, fat 45%, protein 23%)
- Both groups were given intensive instructions on consuming high-quality foods and beverages that were to achieve maximal differentiation in intake of fats and carbohydrates between the 2 diet groups
- No explicit instructions for calorie restriction were given
- The study had two other factors. In one factor, genetic variants thought to influence a person's response to different diets (low-carb vs low-fat) were measured and evaluated. In the other factor, diet response based on baseline insulin secretion was measured and evaluated.
Primary outcome: Primary outcome was 12-month weight change and determination of whether there were significant interactions among
diet type and genotype pattern, diet and insulin secretion, and diet and weight loss
Results
| Duration: 12 months | |||
| Outcome | Low-fat | Low-carb | Comparisons |
|---|---|---|---|
| Primary outcome (average weight loss) | 11.6 lbs | 13 lbs | Diff 1.54 lbs, 95%CI [-0.21 to 1.60] |
| Study dropout rate | 21% | 21% | N/A |
| Average calorie intake (baseline) | 2148 kcal/day | 2223 kcal/day | N/A |
| Average calorie intake (6 months) | 1624 kcal/day | 1621 kcal/day | N/A |
| Average calorie intake (12 months) | 1716 kcal/day | 1697 kcal/day | N/A |
|
|||
Findings: In this 12-month weight loss diet study, there was no significant difference in weight change between a healthy low-fat diet vs a healthy low-carbohydrate diet, and neither genotype pattern nor baseline insulin secretion was associated with the dietary effects on weight loss. In the context of these 2 common weight loss diet approaches, neither of the 2 hypothesized predisposing factors was helpful in identifying which diet was better for whom.
RCT
Low-Carb vs Low-Fat Diet for Weight Loss over 2 Years, Annals of Internal Medicine (2010) [PubMed abstract]
- The study enrolled 307 overweight patients
Main inclusion criteria
- Age 18 - 65 years
- BMI 30 - 40
- Body weight < 299 lbs (136 kg)
Main exclusion criteria
- Type 2 diabetes
- Taking weight loss medications
- Taking lipid-lowering medications
- BP > 140/90 mmHg
Baseline characteristics
- Average age 45 years
- Female - 68%
- Average BMI - 36
- Average weight - 227 lbs (103 kg)
- Average BP - 124/75
- Average LDL - 122 mg/dl
- Average HDL - 46 mg/dl
Randomized treatment groups
- Group 1 (153 patients) - Low-carbohydrate diet
- Diet followed Dr. Atkins' New Diet Revolution plan
- During the first 12 weeks of treatment, participants were instructed to limit carbohydrate intake to 20 grams/day in the form of low–glycemic index vegetables
- After the first 12 weeks, participants gradually increased carbohydrate intake (5 grams/day per week) by consuming more vegetables, a limited amount of fruits, and eventually small quantities of whole grains and dairy products, until a stable and desired weight was achieved
- Group 2 (154 patients) - Low-fat diet
- Limit calorie intake to 1200 - 1500 calories a day for women, 1500 - 1800 calories a day for men
- 55% of calories from carbs, 30% from fat, and 15% from protein
- All participants received comprehensive, in-person group behavioral treatment throughout the study
Primary outcome: Weight loss at 2 years
Results
| Duration: 2 years | |||
| Outcome | Low-carb | Low-fat | Comparisons |
|---|---|---|---|
| Primary outcome | 13.9 lbs | 16.2 lbs | p=0.41 |
| Weight loss at 3 months | 20.9 lbs | 18.4 lbs | p=0.019 |
| Weight loss at 12 months | 23.9 lbs | 23.8 lbs | p=0.95 |
| Decrease in LDL at 2 years | 4.78 mg/dl | 8.01 mg/dl | p=0.25 |
| Increase in HDL at 2 years | 7.75 mg/dl | 4.64 mg/dl | p=0.008 |
| Study dropout rate | 42% | 32% | N/A |
Findings: Successful weight loss can be achieved with either a low-fat or low-carbohydrate diet when coupled with behavioral treatment. A low-carbohydrate diet is associated with favorable changes in cardiovascular disease risk factors at 2 years.
RCT
Weight Loss with Diets of Different Fat, Protein, and Carbohydrate Composition, NEJM (2009)
[PubMed abstract]
- A study in the NEJM enrolled 811 overweight adults
Main inclusion criteria
- Age 30 - 70 years
- BMI 25 - 40
Main exclusion criteria
- Diabetes
- Unstable cardiovascular disease
- Use of medications that affect body weight
Baseline characteristics
- Average age 51 years
- Average BMI - 33
- Female sex - 64%
- Average weight - 205 lbs (93 kg)
Randomized treatment groups
- Diet 1 - Low-fat, average-protein (204 patients) - 20% fat, 15% protein, and 65% carbohydrates
- Diet 2 - Low-fat, high-protein (202 patients) - 20% fat, 25% protein, and 55% carbohydrates
- Diet 3 - High-fat, average-protein (204 patients) - 40% fat, 15% protein, and 45% carbohydrates
- Diet 4 - High-fat, high-protein (201 patients) - 40% fat, 25% protein, and 35% carbohydrates
- Participants received continuous dietary counseling via group and individual sessions throughout the study. Daily meal plans were provided.
- Participants were given individual caloric goals that provided a 750 kcal/day deficit
- The study had a 2X2 factorial design that compared the low vs high fat diets and average vs high protein diets
Primary outcome: Weight loss at 2 years
Results
| Duration: 2 years | |||||
| Outcome | High-protein | Average-protein | High-fat | Low-fat | Comparisons |
|---|---|---|---|---|---|
| Primary outcome | 7.9 lbs | 6.6 lbs | 7.2 lbs | 7.2 lbs | p=0.22 for protein | p=0.94 for fat |
|
|||||
Findings: Reduced-calorie diets result in clinically meaningful weight loss regardless of which macronutrients they emphasize
RCT
Low-carb vs Low-fat vs Low Glycemic Index Diets for Energy Expenditure, JAMA (2012) [PubMed abstract]
- A crossover trial in the JAMA enrolled 24 people who were overweight
Main inclusion criteria
- Age 18 - 40 years
- BMI ≥ 27
Main exclusion criteria
- Body weight ≥ 352 lbs (160 kg)
- Diabetes
- Smoker
- Change in body weight +/- 10% within 1 year
Baseline characteristics
- Average age 30 years
- Average BMI - 34
- Average weight - 231 lbs (105 kg)
- Male - 62%
Diets
- Low-fat diet: Carb 60%, Fat 20%, Protein 20%
- Low-glycemic index diet: Carb 40%, Fat 40%, Protein 20%
- Very low-carb (Atkins) diet: Carb 10%, Fat 60%, Protein 30%
- Subjects were first placed on a calorie-restricted diet for 16 weeks where they lost an average of 13.6% of their body weight. Subjects were then randomized to 1 of 3 diets (low-fat, low-glycemic index, very low-carb) for 4 weeks at a time. After 4 weeks on one diet, each subject crossed over to another diet until they had spent 4 weeks on all 3 diets.
- The diets were designed to maintain weight loss meaning calories-in were equal to expected calories burned
- Metabolic rates were measured on each diet using indirect calorimetry and doubly-labeled water (techniques that measure carbon dioxide production as an indirect measure of metabolism)
Primary outcome: Primary outcome was resting energy expenditure (REE),
with secondary outcomes of total energy expenditure (TEE), hormone levels, and metabolic syndrome components
Results
| Duration: 4 weeks on each diet | ||||
| Outcome | Low-fat | Low GI | Low-carb | Comparisons |
|---|---|---|---|---|
| REE | 1576 kcal/day | 1614 kcal/day | 1643 kcal/day | p=0.03 overall |
| TEE | 2812 kcal/day | 2937 kcal/day | 3137 kcal/day | p=0.003 overall |
| Average body weight on each diet | 91.5 kg | 91.1 kg | 91.2 | p=0.80 overall |
|
||||
Findings: Among overweight and obese young adults compared with pre–weight loss energy expenditure, isocaloric feeding following 10% to 15% weight loss resulted in decreases in REE and TEE that were greatest with the low-fat diet, intermediate with the low–glycemic index diet, and least with the very low-carbohydrate diet.
- OBSEffects of Low-Carb vs Low-Fat Diets on Weight Loss and Cardiovascular Risk Factors, Archives of Internal Medicine meta-analysis (2006) [PubMed abstract]
- A meta-analysis in the Archives of IM looked at trials that compared low-fat to low-carb diets
- The analysis included 5 trials that encompassed 447 participants. Only 3 trials reported results at 12 months
- The analysis found the following:
- The low-carb diets lost significantly more weight at 6 months. At 12 months, the difference was not significant
- Difference in weight loss at 6 months (low-carb minus low-fat): 7.3 lbs, 95%CI [11.6 to 3.1]
- Difference in weight loss at 12 months (low-carb minus low-fat): 2.2 lbs, 95%CI [7.7 to -3.3] [38]
- Findings: Low-carbohydrate, non-energy-restricted diets appear to be at least as effective as low-fat, energy-restricted diets in inducing weight loss for up to 1 year. However, potential favorable changes in triglyceride and high-density lipoprotein cholesterol values should be weighed against potential unfavorable changes in low-density lipoprotein cholesterol values when low-carbohydrate diets to induce weight loss are considered.
- OBSComparison of Weight Loss Among Named Diet Programs in Overweight and Obese Adults, JAMA meta-analysis (2014) [PubMed abstract]
- A network meta-analysis in the JAMA looked at randomized controlled trials that compared popular branded diets to alternatives
- Interventions were divided into 1 of 5 groups:
- 1. No diet
- 2. Moderate macronutrient (Biggest Loser, Jenny Craig, Nutrisystem, Volumetrics, Weight Watchers)
- 3. Low-carb (Atkins, South Beach, Zone)
- 4. Low-fat (Ornish, Rosemary Conley)
- 5. Usual care (LEARN diet)
- The primary outcome was weight loss and body mass index at 6- and 12-month follow-up (±3 months for both periods)
- Compared to no diet, the following was seen:
- Weight loss at 6 months: Low-carb diet - 19 lbs, Low-fat diet - 17.5 lbs, Moderate macronutrient diet - 15 lbs (low-carb vs macronutrient, p<0.05; low-carb vs low-fat, p> 0.05)
- Weight loss at 12 months: Low-carb diet - 16 lbs, Low-fat diet - 16 lbs, Moderate macronutrient diet - 12.5 lbs (low-carb vs macronutrient, p<0.05; low-carb vs low-fat, p> 0.05) [35]
- Findings: Significant weight loss was observed with any low-carbohydrate or low-fat diet. Weight loss differences between individual named diets were small. This supports the practice of recommending any diet that a patient will adhere to in order to lose weight.
- Summary
- Studies have consistently found no significant long-term difference in weight loss between low-carb and low-fat diets. In the short-term (up to 6 months), low-carb diets may cause slightly more weight loss, which may be due to water loss, as carbohydrate restriction leads to rapid depletion of muscle glycogen, a hydrophilic polysaccharide that attracts water.
- The energy expenditure study found that low-carb diets conferred a slightly higher resting energy expenditure than low-fat diets, although body weight did not differ significantly.
HCG DIET
- Overview
- HCG (human chorionic gonadotropin) is a hormone released by the placenta in pregnant women. The HCG diet was developed in the 1950s by a British doctor named Simeons, who claimed that HCG injections alleviated hunger and mood problems in patients on very low-calorie diets (500 calories a day), leading to increased compliance and greater weight loss.
- The effects of the HCG diet were evaluated in the small placebo-controlled trial and meta-analysis detailed below
RCT
HCG Injections vs Placebo for Weight Loss, Amer J of Clinical Nutrition (1976) [PubMed abstract]
- The study enrolled 51 overweight women
Main inclusion criteria
- Between 20 and 60 pounds over ideal body weight as defined by Metropolitan Life Insurance Tables
Main exclusion criteria
- Previous treatment with HCG
- Took appetite suppressant within 3 months
- Weight fluctuation of > 10 lbs in previous 3 months
- Taking medications other than estrogens and birth control pills
Baseline characteristics
- Average age 33 years
- Average weight - 166 lbs
Randomized treatment groups
- Group 1 (25 patients) - Intramuscular HCG 125 units daily, 6 days out of the week for a total of 28 injections
- Group 2 (26 patients) - Placebo injection
- All patients were given a 500 calorie/day diet to follow and encouraged to drink 8 - 10 glasses of water daily
Primary outcome: Weight loss at 32 days
Results
| Duration: 32 days | |||
| Outcome | HCG | Placebo | Comparisons |
|---|---|---|---|
| Primary outcome | 15.8 lbs | 15.5 lbs | p>0.05 |
| Percent body weight lost | 9.5% | 9.3% | p>0.05 |
| Study dropout rate | 20% | 19% | N/A |
|
|||
Findings: HCG does not appear to enhance the effectiveness of a rigidly imposed regimen for weight reduction
- RCTThe Effect of HCG in the Treatment of Obesity by Means of the Simeons Therapy, Br J Clin Pharmacol (1995) [PubMed abstract]
- Researchers attempted to perform a meta-analysis on HCG studies in 1995 but were unable to find enough quality studies. Of the fourteen studies that ranked highest in their review, only two had an outcome in favor of the HCG diet.
- The authors concluded that HCG injections did not have a meaningful effect on weight loss [31]
- Summary
- There is no good evidence that HCG enhances weight loss or prevents hunger during dieting
INTERMITTENT FASTING
- Intermittent fasting has become a popular dieting method because it is easy to follow and may lead to reduced calorie intake. The studies below compared intermittent fasting to usual eating with diets that were calorie-restricted, isocaloric, and unrestricted.
RCT
Intermittent Fasting vs Usual Eating With a Calorie-Restricted Diet, NEJM (2022) [PubMed abstract]
- The study enrolled 139 adults with a BMI between 28 and 45
Main inclusion criteria
- Age 18 - 75 years
- BMI 28 - 45
Main exclusion criteria
- Diabetes
- Taking weight-loss medications
Baseline characteristics
- Average age 32 years
- Male sex - 51%
- Average weight - 194 lbs (88 kg)
- Average BMI - 31
- Average calorie intake - 2070 kcal/day
- Average body fat mass - 73 lbs (33 kg)
Randomized treatment groups
- Group 1 (69 patients): Intermittent fasting (instructed to eat between 8AM and 4PM only)
- Group 2 (70 patients): Usual eating (no restriction on when to eat)
- During the 12 months of the trial, the men were instructed to follow a diet of 1500 to 1800 kcal/day and the women to follow a diet of 1200 to 1500 kcal/day
- Both diets included a combination of 40 - 55% of calories from carbohydrates, 15 - 20% from protein, and 20 - 30% from fat
- Participants were provided with one protein shake (Nutriease) per day for the first 6 months to help improve adherence to the permitted calorie intake
- All participants received dietary counseling
Primary outcome: Difference between the two groups in the change from baseline in body weight at 12 months
Results
| Duration: 12 months | |||
| Outcome | Intermittent fasting | Usual eating | Comparisons |
|---|---|---|---|
| Primary outcome (12 months) | -17.6 lbs (8 kg) | -13.9 lbs (6.3 kg) | p=0.11 |
| Weight loss (6 months) | -20.7 lbs (9.4 kg) | -19.6 lbs (8.9 kg) | N/A |
| Body fat mass (12 months) | -13 lbs (5.9 kg) | -10 lbs (4.5 kg) | N/A |
| Adherence | 84% | 83% | N/A |
|
|||
Findings: Among patients with obesity, a regimen of time-restricted eating was not more beneficial with regard to reduction in body weight, body fat, or metabolic risk factors than daily calorie restriction.
- RCTIntermittent Fasting vs Usual Eating with a Calorie-Restricted Diet, JAMA Intern Med (2022) [PubMed abstract]
- Design: Randomized, controlled trial (N=90 | length = 14 weeks) in obese adults (average BMI 39.6)
- Treatment: Intermittent fasting (8-hour eating window from 7:00 to 15:00) vs Eating over a window of 12 hours or more (control group). All participants were counseled on consuming an energy-restricted diet.
- Primary outcomes: Weight loss and fat loss
- Results:
- Primary outcome (weight loss): Intermittent fasting - 13.9 lbs, Control - 8.8 lbs (p=0.002)
- Primary outcome (fat loss): Intermittent fasting - 10.3 lbs, Control - 7.5 lbs (p=0.09)
- Findings: In this randomized clinical trial, early time-restricted eating was more effective for losing weight and improving diastolic blood pressure and mood than eating over a window of 12 or more hours at 14 weeks.
- RCTIntermittent Fasting for 3 Days a Week vs Usual Eating with a Calorie-Restricted Diet, Ann Intern Med (2025) [PubMed abstract]
- Design: Randomized, open-label trial (N=165 | length = 12 months) in adults aged 18 to 60 years with a BMI of 27 to 46
- Treatment: 4:3 intermittent fasting (IMF) with 80% energy restriction on 3 nonconsecutive days per week and ad libitum intake on the other 4 days vs Daily caloric restriction (DCR) with a 34% reduction in daily energy intake
- Primary outcome: Change in body weight (in kilograms) at 12 months
- Results:
- Primary outcome (weight loss): IMF - 17 lbs (7.7 kg), DCR - 10.5 lbs (4.8 kg) (P=0.040)
- Findings: Compared with DCR, 4:3 IMF resulted in modestly greater weight loss among adults with overweight or obesity enrolled in a 12-month, high-intensity, comprehensive behavioral weight loss program
- RCTIntermittent Fasting vs Usual Eating for Weight Loss in Overweight Individuals, JAMA Intern Med (2020) [PubMed abstract]
- Design: Randomized controlled trial (N=116 | length = 12 weeks) in adults with a BMI of 27 - 43
- Treatment: Intermittent fasting (no calories from 8PM to 12PM the following day) vs Usual eating. No recommendations on calorie intake or physical activity were given.
- Primary outcome: Weight loss at 12 weeks
- Results:
- Primary outcome (weight loss): Intermittent fasting - 2 lbs (0.94 kg), Usual eating - 1.5 lbs (0.68 kg) (p=0.63)
- Findings: Time-restricted eating, in the absence of other interventions, is not more effective in weight loss than eating throughout the day
- RCTIntermittent Fasting vs Usual Eating for Weight Loss in Adults with Obesity and Prediabetes or Diet-controlled Diabetes, Ann Intern Med (2024) [PubMed abstract]
- Design: Randomized controlled trial (N=41 | length = 12 weeks) in obese adults (average BMI 36) with prediabetes or diet-controlled diabetes
- Treatment: Intermittent fasting (10-hour eating window, 80% of calories before 1 p.m.) vs Usual eating (≤ 16-hour window, ≥ 50% of calories after 5 p.m.). Subjects received isocaloric diets with equivalent micro- and macronutrient composition; calorie amounts were based on metabolic needs and activity levels. Food was prepared in a study kitchen and consumed onsite or taken home.
- Primary outcome: Change in body weight at 12 weeks
- Results:
- Baseline weight: Intermittent fasting - 210 lbs (95.6 kg), Usual eating - 228 lbs (103.7 kg)
- Primary outcome (weight loss): Intermittent fasting - 5.1 lbs (2.3 kg), Usual eating - 5.7 lbs (2.6 kg) (diff 0.3 kg, 95%CI [-1.2 to 1.9 kg])
- Findings: In the setting of isocaloric eating, intermittent fasting did not decrease weight or improve glucose homeostasis relative to usual eating, suggesting that any effects of intermittent fasting on weight in prior studies may be due to reductions in caloric intake.
- RCTIntermittent Fasting vs Calorie Restriction vs Usual Eating, Ann Intern Med (2023) [PubMed abstract]
- Design: Randomized controlled trial (N=90 | length = 12 months) in racially-diverse obese adults
- Treatment: Intermittent fasting (eating between noon and 8 PM) vs Calorie-restricted diet (25% energy restriction daily) vs Usual eating (control)
- Primary outcome: Change in body weight, metabolic markers, and energy intake by month 12
- Results:
- Percent weight reduction (difference from control): Intermittent fasting - 4.87%, Calorie restriction - 5.3%
- Mean calorie reduction: Intermittent fasting - 425 kcal/d, Calorie restriction - 405 kcal/d
- Both interventions were significantly better than control. There was no significant difference between intermittent fasting and calorie restriction.
- Findings: Time-restricted eating is more effective in producing weight loss when compared with control but not more effective than calorie restriction in a racially diverse population.
- Summary
- Intermittent fasting did not enhance weight loss in four studies and had a modest effect in two. Long-term adherence to the time constraints seems impractical, making it a fad diet for most.
WEIGHT LOSS MEDICATIONS
- Overview
- See weight loss drugs below for a list of FDA-approved therapies. Plenity®, an oral capsule, is also available, but the FDA considers it an "ingested, transient, space-occupying device."
- Weight loss procedures are reviewed here - weight loss procedures
- The table below ranks medications and procedures by their effectiveness
| Average weight loss for obesity treatments | |
|---|---|
| Treatment | % weight loss from baseline (length of follow-up) |
| BPD/DS | 35 - 40% (> 10 years) |
| Gastric bypass | 30 - 35% (> 10 years) |
| Gastric sleeve | 25 - 30% (> 10 years) |
| Gastric banding | 20 - 25% (> 10 years) |
| Zepbound (tirzepatide) | 21% (72 weeks) |
| Wegovy (semaglutide) | 16% (68 weeks) |
| Endoscopic sleeve gastroplasty | 11.4% (104 weeks) |
| Intragastric balloon | 10% (6 months) |
| Appetite suppressants (e.g. phentermine) | 10% (6 months) |
| Qsymia (topiramate + phentermine) | 10% (56 weeks) |
| Saxenda (Liraglutide) | 8% (56 weeks) |
| Xenical (orlistat) | 7.6% (2 years) |
| Plenity (hydrogel) | 6.4% (24 weeks) |
| Contrave (naltrexone + bupropion) | 6.1% (56 weeks) |
- Weight loss medication classes
- Appetite suppressants
- Benzphetamine (Didrex®)
- Diethylpropion HCL (Tenuate®)
- Phendimetrazine (Bontril® PDM)
- Phentermine HCL (Adipex-P®)
- Contrave® (bupropion + naltrexone)
- GLP-1 drugs
- Lipase inhibitors (orlistat)
- Xenical®
- Alli®
- Qsymia® (topiramate + phentermine)
PLENITY®
- NOTE: the Plenity manufacturer, Gelesis, filed for bankruptcy in October 2023, and it is unclear if Plenity is still available.
- Mechanism of action
- Plenity capsules contain particles of a nonsystemic superabsorbent hydrogel composed of cellulose and citric acid. After ingestion, the particles are released in the stomach, where they absorb 100 times their original weight, forming a gel that occupies a quarter of the space. During a meal, the gel mixes with ingested food to increase its volume, enhancing fullness and satiety. The gel then passes through the small intestine and into the colon, where it is degraded before being eliminated in the stool. See YouTube video on how Plenity works.
- Despite its capsule form, Plenity is considered a medical device by the FDA, which describes it as an "ingested, transient, space occupying device for weight management and/or weight loss."
- FDA-approved indication
- Plenity is approved as an aid in weight management in overweight and obese adults, with a BMI of 25 - 40 kg/m2, when used in conjunction with diet and exercise
- Side effects
- Plenity side effects include diarrhea (13%), abdominal distension (12%), infrequent bowel movements (9%), flatus (9%), and abdominal pain (5%). See GLOW study below.
- Contraindications / Precautions
- Pregnancy - DO NOT USE
- History of allergy to cellulose, citric acid, sodium stearyl fumarate, gelatin, or titanium dioxide - DO NOT USE
- Esophageal anatomic anomalies, including webs, diverticuli, and rings - DO NOT USE
- Suspected strictures (such as patients with Crohn's disease) - DO NOT USE
- Complications from prior gastrointestinal (GI) surgery that could affect GI transit and motility - DO NOT USE
- Gastro-esophageal reflux disease (GERD), ulcers, or heartburn - use caution. May worsen symptoms.
- Drug interactions
- Plenity is not absorbed so it does not have systemic drug interactions, but the gel it forms could theoretically affect drug absorption. A study evaluating its effects on metformin absorption found that while absorption was decreased, the effect was no different than that of food.
- The Plenity prescribing information offers no real guidance on administering concomitant medications. Based on the metformin study, it can be assumed that Plenity has a similar effect as food, although this has not been studied extensively.
- In general, patients should try to take their medications 1 hour before or 4 hours after Plenity when possible
- Dosage form
- Plenity comes in a pod that contains 3 capsules. Fourteen pods equal a week's worth of treatment.
- Plenity is only available from a mail-order pharmacy called GoGoMeds. A four-week supply costs $98.
- NOTE: the Plenity manufacturer, Gelesis, filed for bankruptcy in October 2023, and it is unclear if Plenity is still available.
- Dosing
- Dosing: 3 capsules (1 pod) 20 - 30 minutes before lunch and dinner. For each dose, patients should follow these steps:
- 1. Swallow 3 capsules with water
- 2. After taking the capsules, drink 2 additional glasses of water (8 fl oz/250 ml each)
- 3. Wait 20 - 30 minutes to begin to eat
- If a dose is missed, Plenity can be taken during or immediately after a meal
RCT
GLOW study - Plenity vs Placebo for Weight Loss in Overweight Patients, Obesity (2019) [PubMed abstract]
- The GLOW study enrolled 436 adults with a BMI of 27 - 40.
Main inclusion criteria
- Age 22 - 65 years
- BMI 27 - 40
- Fasting blood sugar 90 - 145 mg/dl
Main exclusion criteria
- Type 1 diabetes
- History of eating disorder
- Significant GI disorder
- Gastric bypass or other GI surgery
- Required to take meds with meals
Baseline characteristics
- Average age 48 years
- Average weight - 218 lbs (99 kg)
- Average BMI - 34
- Type 2 diabetes - 10%
Randomized treatment groups
- Group 1 (223 patients): Plenity 3 capsules 20 to 30 minutes before lunch and dinner
- Group 2 (213 patients): Placebo
- All patients were prescribed a hypocaloric diet of 300 kcal/d below their calculated energy requirement (with 45% to 50% of daily calorie intake from carbohydrates, ≤ 30% from fat, and 20% to 25% from protein)
- All patients were instructed to perform daily moderate-intensity exercise (e.g. 30 minutes of walking/day) and maintain their smoking habits during the study
Primary outcome: The co-primary efficacy endpoints were the percent change in body weight from baseline (visit 2) to day 171 (visit 13) and the percent of patients who lost ≥ 5% body weight from baseline to day 171
Results
| Duration: 24 weeks | |||
| Outcome | Plenity | Placebo | Comparisons |
|---|---|---|---|
| Percent change in body weight | -6.4% | -4.4% | p=0.0007 |
| ≥ 5% weight loss | 59% | 42% | p=0.0008 |
| ≥ 10% weight loss | 27% | 15% | p=0.0107 |
| Study dropout rate | 23% | 29% | N/A |
| Diarrhea | 12.6% | 8.5% | p=0.21 |
| Abdominal distension | 11.7% | 6.6% | p=0.09 |
| Infrequent bowel movements | 9.4% | 4.7% | p=0.064 |
| Flatulence | 8.5% | 5.2% | p=0.19 |
| Abdominal pain | 5.4% | 2.8% | p=0.23 |
| Constipation | 5.4% | 5.2% | p=1.0 |
| Dyspepsia | 4% | 0.9% | p=0.063 |
Findings: Gelesis100 is a promising new nonsystemic therapy for overweight and obesity with a highly
desirable safety and tolerability profile
- Summary
- Plenity is a new "medical device" that may help some people lose weight by increasing food satiety. Based on the results of the GLOW study, a person who weighs 218 pounds can expect to lose an additional 4.4 pounds over 24 weeks if they add Plenity to diet and exercise.
MACRONUTRIENTS
BIBLIOGRAPHY
- 1 - PMID 20089729
- 2 - PMID 19116329
- 3 - PMID 19190072
- 4 - PMID 19299006
- 5 - PMID 21121834
- 6 - PMID 16403931
- 7 - PMID 10933273
- 8 - PMID 15616204
- 9 - PMID 17986696
- 10 - PMID 17395851
- 11 - PMID 11343442
- 12 - PMID 10511607
- 13 - PMID 18239557
- 14 - PMID 12499325
- 15 - PMID 19720791
- 16 - PMID 19246357
- 17 - PMID 17976244
- 18 - PMID 20679559
- 19 - PMID 19615091
- 20 - PMID 19439458
- 21 - PMID 19366978
- 22 - PMID 18635428
- 23 - PMID 18175733
- 24 - PMID 16770923
- 25 - PMID 20679559
- 26 - PMID 786001
- 27 - PMID 2405506
- 28 - PMID 595585
- 29 - PMID 792477
- 30 - PMID 4574032
- 31 - PMID 8527285
- 32 - PMID 17636786
- 33 - PMID 16864756
- 34 - PMID 17507345
- 35 - PMID 25182101
- 36 - PMID 25182100
- 37 - SSED for dual intragastric balloon
- 38 - PMID 16476868 - AIM MA on low-carb vs low-fat
- 39 - AspireAssist SSED on FDA website
- 40 - PMID 33832655 AGA Clinical Practice Guidelines on Intragastric Balloons in the Management of Obesity, Gastroenterology (2021)
