Acronyms and definitions
- ADA - American Diabetes Association
- Basal insulin - Long- and intermediate-acting insulins used to supply constant levels of insulin activity over the course of a day
- Carb - Carbohydrate
- T1DM - Type 1 diabetes
- T2DM - Type 2 diabetes
- Multidose insulin regimen - Insulin regimens that include both basal and premeal insulins
- Prandial insulin - Rapid and short-acting insulins given at mealtime
- Premeal insulin - also called “prandial” insulin. Rapid and short-acting insulins given at mealtime.
- Total daily dose of insulin - Sum in units of premeal and basal insulin given in a day
- 1 kilogram = 2.2 pounds
IMPORTANT POINTS ABOUT DOSING INSULIN
- Overview
- There are many different ways to dose insulin, and no single regimen fits every patient. Patient variables, including education, motivation, diabetes control, and resources, must all be considered when determining which method works best for each individual.
- Low blood sugar (Hypoglycemia)
- In most patients, the main concern when initiating insulin is the risk of hypoglycemia. To help lower the risk, blood sugar monitoring should be increased, and all patients should be aware of the signs, symptoms, and treatment of hypoglycemia (see hypoglycemia for more).
- Measures to help prevent low blood sugars
- Insulin-naïve patients should start at the lower end of dosing ranges and titrate slowly
- Patients should try to avoid insulin doses outside of their prescribed regimens as this may lead to incorrect adjustments
- Patients should attempt to consume a consistent diet of three meals a day while keeping meals as uniform as possible in size and carbohydrate content. Patients should notify their provider and increase monitoring if they decide to make significant changes to their diet (e.g. start a keto diet, drastically reduce calorie intake).
- When using a multidose regimen (basal and premeal), adjust one regimen at a time and alternate between the two (see alternating regimens for more)
INSULIN CATEGORIES
- For dosing purposes, insulins can be divided into two categories:
- Basal insulins - basal insulins provide a steady amount of background insulin activity over the course of a day
- Premeal insulin (prandial insulin) - premeal insulins provide a burst of insulin that acts quickly to abate the rise in blood glucose that is seen after consuming a meal
- See insulin chart for a review of available insulins including their pharmacokinetics, dosage forms, storage, and more
- Basal insulins
- Intermediate-acting insulins
- Humulin® N (NPH)
- Novolin® N (NPH)
- Long-acting insulins
- Basaglar® (insulin glargine)
- Lantus® (insulin glargine)
- Levemir® (insulin detemir)
- Rezvoglar® (insulin glargine)
- Semglee® (insulin glargine)
- Toujeo® (insulin glargine)
- Tresiba® (insulin degludec)
- Premeal insulins
- Rapid-acting insulins
- Admelog® (insulin lispro)
- Afrezza® (inhaled insulin)
- Apidra® (insulin glulisine)
- Fiasp® (insulin aspart)
- Humalog® (insulin lispro)
- Lyumjev® (insulin lispro-aabc)
- Novolog® (insulin aspart)
- Short-acting insulins
- Humulin® R (regular)
- Novolin® R (regular)
BLOOD SUGAR GOALS
TYPE 1 DIABETES INSULIN RECOMMENDATIONS
- ADA general treatment recommendations for T1DM
- T1DM patients should receive multidose injections (3 - 4 a day) of basal and premeal insulin or insulin pump therapy
- Most individuals with T1DM should use rapid-acting insulin analogs to reduce hypoglycemia risk
- Patients should match premeal insulin to carbohydrate intake, premeal blood glucose levels, and anticipated activity [26]
- Starting therapy
- Insulin dosing in T1DM will vary based on patient's age, weight, and residual pancreatic insulin activity
- T1DM patients will typically require a total daily insulin dose of 0.4 - 1.0 units/kg/day
- A typical starting dose in metabolically-stable patients is 0.5 units/kg/day
- After calculating the total daily dose, it should be given as follows:
- Basal insulin - given as half of the total daily dose ✝
- Premeal insulin - half of the total daily dose divided into thirds and given before each meal
- ✝ When first starting therapy, it is recommended that the initial basal dose be reduced by 20 - 30% to prevent hypoglycemia [11,19]
- T1DM patients may experience a "honeymoon phase" after starting insulin therapy where the initial effects of insulin are greater than what is seen later in the disease [7,13,26]
- Example
- Patient weighs 80 kg
- Total daily dose = 80 kg X (0.5 units/kg/d) = 40 units per day
- Basal insulin = 1/2 X 40 units = 20 units of basal per day✝
- Premeal Insulin = 1/2 X 40 units = 20 units / 3 = approximately 7 units before each meal
- ✝ If patient is just starting therapy, the initial basal dose should be reduced by 20 - 30%. In our example: 20 units X 0.20 = 4 units, so initial basal dose would be 20 - 4 = 16 units
- Adjusting therapy
- See adjusting basal insulin and adjusting premeal insulin below
TYPE 2 DIABETES INSULIN RECOMMENDATIONS
| ADA Insulin Dosing Recommendations for Adults with T2DM |
|---|
Step 1 - start with long-acting insulin or bedtime NPH
|
Step 2 - add premeal insulin before largest meal
|
Step 3 - add premeal insulin before other meals in stepwise fashion
|
| ADA Insulin Recommendations for Youth with T2DM |
|---|
Basal insulin
|
| ADA Insulin Recommendations for Elderly with T2DM |
|---|
Overview
|
Basal insulin
|
|
Premeal (prandial) insulin
|
ADJUSTING BASAL INSULIN
- Overview
- ADA basal insulin recommendations for T2DM are provided above (see ADA T2DM insulin recommendations). The three-day method discussed below can be used in type one and type two diabetes and has been proven effective in clinical trials.
- When NPH is used as the basal insulin, other considerations should be taken into account. See NPH dosing for more.
- Three-day method for adjusting basal insulin
- 1. Measure fasting blood sugar (no calories for 8 hours) for previous three consecutive days
- 2. Calculate the average of the three fasting blood sugars
- 3. Adjust basal insulin dose based on the table below
- 4. Repeat steps 1-3 until target range (80 - 99) is achieved
| Fasting blood sugar (mg/dl) average over 3 days |
Adjustment to basal insulin dose (units of insulin) |
|---|---|
| ≥ 180 | add 8 units |
| 160 - 179 | add 6 units |
| 140 - 159 | add 4 units |
| 120 - 139 | add 2 units |
| 100 - 119 | add 1 unit |
| 80 - 99 | no change |
| 60 - 79 | subtract 2 units |
| < 60 | subtract 4 or more units |
ADJUSTING PREMEAL INSULIN
- Overview
- There are several ways to adjust premeal insulin. The scale method and the carb counting method are detailed below. These methods are appropriate for type 1 diabetics and highly-motivated type 2 diabetics. ADA recommendations for type 2 diabetics are presented above (see ADA T2DM insulin recommendations).
- Scale method
- With the scale method, premeal insulin is adjusted based on a scale
- Patients should try to consume the same amount of carbohydrates at each meal (a typical amount is about 60 grams a meal and 15 grams for a bedtime snack)
- Carbohydrate goals vary by individual (see carbohydrate information below)
- Steps:
- 1. Measure blood sugar fasting (pre-breakfast), pre-lunch, pre-dinner, and pre-bedtime snack for previous three consecutive days
- 2. Average the pre-lunch, pre-dinner and pre-bedtime values separately
- 3. Adjust the premeal insulin dose based on the table below
- 4. Repeat steps 1-3 until target range is achieved
- 5. A Correction Factor (see below) should also be incorporated when blood sugars are checked
|
|
| Premeal blood sugar (mg/dl) average over 3 days |
Adjustment to premeal insulin dose |
|---|---|
| ≥ 180 | add 3 units |
| 160 - 179 | add 2 units |
| 140 - 159 | add 2 units |
| 120 - 139 | add 1 units |
| 100 - 119 | maintain dose (desired range) |
| 80 - 99 | subtract 1 unit |
| 60 - 79 | subtract 2 units |
| < 60 | subtract 4 or more units |
ADJUSTING PREMEAL INSULIN (CARBOHYDRATE COUNTING)
- Carbohydrate counting
- In carbohydrate counting, premeal insulin is adjusted based on the amount of carbohydrates to be consumed in each meal
- The carbohydrate counting method is used to determine the amount of carbohydrates in a meal
- An insulin to carbohydrate ratio (ex. 1 unit/10g of carb) is used to calculate the premeal insulin dose
- A typical starting ratio is 1 unit of premeal insulin for every 10 grams of carbs to be consumed
- An individual may have different carbohydrate ratios for breakfast, lunch, and dinner because a person's response to insulin may vary throughout the day
- Example:
- 60 grams of carbs to be consumed for lunch
- Patient's ratio is 1 unit of insulin for every 10 grams of carbs
- Patient injects 6 units of premeal insulin before eating meal
- Steps for adjusting an insulin-to-carb ratio
- 1. Calculate the number of carbs to be consumed in a meal using carbohydrate counting
- 2. Dose premeal insulin based on number of carbs in a meal (typical starting point is 1 unit of premeal insulin for every 10 grams of carbs)
- 3. Measure blood sugar fasting (pre-breakfast), pre-lunch, pre-dinner, and pre-bedtime snack for previous three consecutive days
- 4. Average the pre-lunch, pre-dinner and pre-bedtime snack blood sugar values separately
- 5. Adjust the carbohydrate to insulin ratio as instructed in the table below
- 6. Repeat steps 1-5 until appropriate ratios are determined [3,4]
- 7. A Correction Factor (see below) should also be incorporated when blood sugars are checked
|
|
If average blood sugar is > 120 mg/dl, adjust ratio by subtracting 2 - 3g of carbohydrate
|
|
If average blood sugar is < 80 mg/dl, adjust ratio by adding 2 - 3g of carbohydrate
|
| If average blood sugar is 80 - 120 mg/dl, do not adjust ratio |
ADJUSTING PREMEAL AND BASAL INSULINS CONCURRENTLY
- Overview
- When adjusting premeal and basal insulins concurrently, adjustments to one regimen may affect the other. This can lead to overcorrections and hypoglycemia. Alternating between regimens can help to prevent these issues.
- Example:
- Day 3 - adjust basal
- Day 6 - adjust premeal
- Day 9 - adjust basal
- Day 12 - adjust premeal, and so on...
CORRECTION FACTOR
- Overview
- When premeal blood sugar checks are high, a correction factor should be used with premeal insulin
- The correction factor supplies supplemental insulin to account for the elevated blood sugar
- Insulin used in the correction factor should not be included in calculations for adjusting premeal or basal insulin
- There are several methods for determining the correction factor. The flat method uses a simple ratio, and the individual method incorporates the patient's total daily insulin dose.
- When initiating therapy, the flat method is preferred since the appropriate total daily insulin dose will be unknown
- Flat method
- One unit of insulin is added to the premeal dose for every 25 mg/dl that the blood sugar is above the upper limit of the desired range
- Example:
- Pre-lunch blood sugar is 200 mg/dl
- Upper limit of desired range is 120 mg/dl
- 200 - 120 = 80 mg/dl above desired range
- 80 mg/dl ÷ 25 mg/dl = approximately 3
- Add 3 extra units to premeal dose
- Individual method
- The individual method uses a patient's total daily insulin dose to calculate a correction factor
- The correction factor is calculated differently for regular insulins (Humulin R, Novolin R) and rapid insulins (Novolog, Humalog, Apidra, Fiasp)
|
Step 1 - calculate the correction factor
|
|
Step 2 - Once the correction factor is calculated, the patient can then figure out how much insulin to supplement
|
NPH DOSING
- NPH properties
- NPH insulin is an intermediate-acting insulin that can be used as a basal insulin. Newer long-acting insulin analogs have largely supplanted NPH as first-line basal insulins, but NPH remains the most affordable insulin available at $25/vial and is, therefore, still an important option for patients without insurance and/or those who are cost-sensitive.
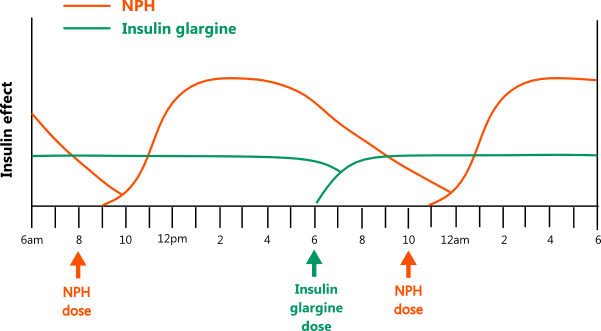
- When using NPH, it's essential to understand how its pharmacokinetic properties differ from other basal insulins. Long-acting insulins provide a steady state of insulin that does not have a peak. NPH insulin has a peak effect that occurs between 4 - 10 hours after dosing. Because of this, NPH carries a higher risk of hypoglycemia. In addition, NPH's duration of effect is around 16 - 20 hours, which is shorter than the 24+ hours seen with long-acting insulins. This means NPH often has to be dosed twice daily to achieve sustained control over 24 hours.
- The diagram below illustrates the different pharmacokinetics of NPH and long-acting insulins [11,29]
- Important points about NPH dosing
- NPH is a suspension, and it must be resuspended before dosing. Failure to resuspend NPH properly can result in dosing irregularities. The vials and the pens contain directions on how to resuspend each product. NPH should appear uniformly white and cloudy after proper resuspension.
- Since NPH has a peak effect, patients should keep the timing of their injections and meals consistent to help prevent hypoglycemia. Patients should also try to consume meals that are uniform in size and carbohydrate content.
- Patients who are also using premeal insulins should be aware that NPH may potentiate the effect of their premeal insulin. For example, a patient who injects NPH and a rapid-acting insulin before breakfast will see a peak effect from the rapid insulin around 1 - 3 hours after injection. The NPH will start to have its effect around 2 - 3 hours after injection, and the combined peak actions may lead to hypoglycemia. More frequent blood sugar checks and/or dose adjustments may be necessary when initiating therapy.
- In the evening, NPH should typically be dosed at bedtime (as opposed to dinner), as this has been shown to decrease the incidence of nighttime hypoglycemia [11,28]
- Twice-daily NPH
- Twice-daily NPH regimens divide the daily dose between a morning and evening dose. In studies, dose distribution has varied widely, with some splitting the dose 50-50, some giving 2/3 in the morning and 1/3 in the evening, and others giving 1/3 in the morning and 2/3 in the evening. [30,31,32,33,34,35]
- The steps below are derived from clinical trials and guidelines. They are intended to provide a starting point for initiating and adjusting twice-daily NPH in type 2 diabetics. The recommendations should be individualized as some patients may require more aggressive adjustments (e.g. poorly-controlled morbidly obese diabetics), and others may need minor adjustments (e.g. elderly, hypoglycemia concerns). For recommendations in patients who are switching from another insulin to NPH, see converting from other insulins to NPH below.
| Dosing NPH Insulin in T2DM | ||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Step 1 - Initial dose
|
||||||||||||||||||||||||||||||||||||||||||||
Step 2 - Monitor blood sugars
|
||||||||||||||||||||||||||||||||||||||||||||
Step 3 - Determine insulin adjustment
|
||||||||||||||||||||||||||||||||||||||||||||
Step 4 - Distributing the insulin adjustment
|
||||||||||||||||||||||||||||||||||||||||||||
- Twice-daily NPH example:
- Patient initiates NPH insulin at 10 units twice daily
- Patient blood sugar readings from 3 consecutive days are as follows:
- Fasting: 185, 133, 156
- Predinner: 256, 300, 190
- Average of all blood sugars = (185 + 133 + 156 + 256 + 300 + 190) / 6 = 203
- Based on table in Step 3, patient will add 8 units to the total daily NPH dose
- Average of fasting blood sugars is = (185 + 133 + 156)/3 = 158
- Average of predinner blood sugars is = (256 + 300 + 190)/3 = 249
- Based on tables in Step 4, fasting blood sugars are range 2, and predinner blood sugars are range 3
- Based on dose distribution table in Step 4, patient will add 67% of the 8 additional units to his morning dose and 33% to the bedtime dose
- 67% of 8 = 0.67 X 8 = 5.36 rounded down to 5 units
- 33% of 8 = 0.33 X 8 = 2.64 rounded up to 3 units
- Patient's new NPH dose is 15 units in the morning and 13 units at night
- Once-daily NPH
- The ADA guidelines list once-daily bedtime NPH as an option in type 2 diabetics (see ADA T2DM insulin recommendations). Patients with normal fasting AM blood sugars may want to give their NPH dose in the morning instead of night.
- Once-daily dosing may work for some people, but others may require twice-daily NPH to reach their goals.
- Converting from long-acting insulins to NPH
- When converting from long-acting insulins to NPH, patients should know how NPH properties differ and review important points about NPH dosing.
- In trials with type 1 diabetics who were switching from other basal insulins to NPH and vice versa, the total daily basal insulin dose was reduced by 25 - 30% upon initiation. This approach helps prevent hypoglycemia but may require significant up-titration after switching. Patients who are also receiving premeal insulin should be particularly cautious because NPH may potentiate the peak effect of short-acting insulins.
- Recommendations from manufacturers for converting between NPH and other insulins are provided below (see converting between insulin brands and types) [11]
- Dosing 70/30 insulin
- Novolin 70/30 and Humulin 70/30 contain 70% NPH and 30% regular insulin. Insulin mixes like 70/30 are more difficult to adjust because the premeal and basal insulin must be given simultaneously and in a 7:3 ratio. Given these constraints, insulin mixes are not widely used anymore.
- In studies with type 2 diabetics, 70/30 has typically been initiated at doses of 0.2 - 0.6 units/kg/day, with two-thirds of the daily dose given before breakfast and one-third before dinner. The daily dose can then be adjusted up or down in increments of 10%, depending on blood sugar readings. [34,35]
SLIDING SCALE INSULIN
- Sliding scale insulin is rapid or short-acting insulin doses given to treat elevated blood sugar readings. The insulin dose is based on the glucose value.
- Different scales can be used depending on the patient and their insulin sensitivity. The example below is a typical starting point.
| Blood sugar (mg/dl) | Insulin dose in units of rapid or short-acting |
|---|---|
| < 150 | 0 |
| 150 - 200 | 2 |
| 201 - 250 | 4 |
| 251 - 300 | 6 |
| 301 - 350 | 8 |
| 351 - 400 | 10 |
| 401 - 450 | 12 |
| > 450 | 14 |
CONVERTING BETWEEN INSULIN BRANDS AND TYPES
- Overview
- Caution should be exercised when converting between insulin products because glucose effects may vary between individuals. Insulin manufacturers make some recommendations, but they do not cover every scenario, and there are few trials directly comparing the effects of different insulins.
- When switching, patients at high risk for hypoglycemia should reduce their daily basal insulin dose by 20 - 30% and re-titrate. All patients should increase blood sugar monitoring until they know how the new insulin will affect them.
| Converting between insulin brands and types |
|---|
Rapid-acting and short-acting insulin
|
Lantus, Basaglar, Levemir, and Tresiba
|
|
Lantus/Basaglar ⇄ NPH
|
|
Lantus/Basaglar ⇄ Toujeo
|
|
Levemir and NPH
|
|
Levemir and Toujeo
|
|
Toujeo and NPH
|
|
Toujeo and Tresiba
|
|
Tresiba and NPH
|
CARBOHYDRATE INFORMATION
- Carbohydrates and insulin
- Carbohydrates have the most direct effect on blood sugars; therefore, patients receiving insulin should monitor their intake and understand their properties. Extensive information on carbohydrates is available at the links below.
- Carbohydrate counting - review of carbohydrate counting used in dosing premeal insulin
- Glycemic index - a method of determining the effects of different foods on blood sugars
- Carbohydrates - review of the different types of carbohydrates found in foods
- Calories - review on calculating caloric requirements
- Diabetic diet - diabetic diet recommendations
BIBLIOGRAPHY
- 1 - PMID 18945920
- 2 - PMID 10332663
- 3 - PMID 18364392
- 4 - Braithwaite S: Case Study: Five Steps to Freedom: Dose Titration for Type 2 Diabetes Using Basal-Prandial-Correction Insulin Therapy. Clinical Diabetes Vol 23:1 p39-43 2005
- 5 - Kulkarni K: Carbohydrate Counting: A Practical Meal-Planning Option for People With Diabetes. Clinical Diabetes Vol 23:3 p120-122 2005
- 6 - PMID 16915796
- 7 - PMID 15616254
- 8 - PMID 16921608
- 9 - PMID 10378067
- 10 - PMID 21193625
- 11 - PMID 12734137 - Outpatient Insulin Therapy in Type 1 and Type 2 Diabetes Mellitus, JAMA (2003)
- 12 - PMID 16847295
- 13 - Herbst K, Hirsch I Insulin Strategies for Primary Care Providers. Clinical Diabetes. Vol 20:1 p1-7 2002
- 14 - PMID 17890232 - NEJM DM 2 study
- 15 - Hirsch I et al. A Real-World Approach to Insulin Therapy in Primary Care Practice. Clinical Diabetes. Vol 23:2 p78-86. 2005
- 16 - PMID 18165339
- 17 - PMID 12766131
- 18 - Glucagon PI
- 19 - Lantus PI
- 20 - Levemir PI
- 21 - Toujeo PI
- 22 - Tresiba PI
- 23 - Basaglar PI
- 24 - ADA 2015 Standards of Medical Care in Diabetes, Vol 38, Supplement 1, p. S46
- 25 - PMID 29222370 - ADA 2018 Standards of Medical Care in Diabetes
- 26 - ADA 2019 Standards of Medical Care in Diabetes
- 27 - ADA 2020 Standards of Medical Care in Diabetes
- 28 - PMID 11926785 - Administration of neutral protamine Hagedorn insulin at bedtime versus with dinner in type 1 diabetes mellitus to avoid nocturnal hypoglycemia and improve control. A randomized, controlled trial, Ann Intern Med (2002)
- 29 - PMID 16160867 - Pharmacokinetic and glucodynamic variability: assessment of insulin glargine, NPH insulin and insulin ultralente in healthy volunteers using a euglycaemic clamp technique, Diabetologia (2005)
- 30 - PMID 16732007 - A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes, Diabetes Care (2006)
- 31 - 15298338 - Insulin analogues (insulin detemir and insulin aspart) versus traditional human insulins (NPH insulin and regular human insulin) in basal-bolus therapy for patients with type 1 diabetes, Diabetologia (2004)
- 32 - PMID 15111525 - Insulin detemir offers improved glycemic control compared with NPH insulin in people with type 1 diabetes: a randomized clinical trial, Diabetes Care (2004)
- 33 - PMID 11092282 - Appropriate Insulin Regimens for Type 2 Diabetes, Diabetes Care (2000)
- 34 - PMID 12882841 - Beneficial effects of insulin versus sulphonylurea on insulin secretion and metabolic control in recently diagnosed type 2 diabetic patients, Diabetes Care (2003)
- 35 - PMID 27278922 - Biphasic insulin Aspart 30 vs. NPH plus regular human insulin in type 2 diabetes patients; a cost-effectiveness study, BMC Endocr Disord (2016)
- 36 - ADA 2023 Standards of Medical Care in Diabetes, Diabetes Care (2023)
